Addressing infant and early childhood mental health needs: opportunities for community solutions
Report • Oct 13, 2021

Report • Oct 13, 2021

Summary
This report delves into the historical and escalating mental health needs of very young children, the current landscape, and the ways in which California, local agencies, and communities must bolster their support and resources in the wake of the pandemic and its potential impacts on child development. This paper focuses specifically on community-based programs in California supporting infants, toddlers, and preschoolers’ social-emotional health, as well as their goals, service models, and funding sources.
Table of Contents
Prevalence and types of programs
California’s children and families are under significant and escalating toxic stress, from both the COVID-19 pandemic and longstanding historical and systemic issues such as poverty, racism and other forms of community and individual trauma.
This moment in history could be pivotal in the landscape of California’s early childhood mental health. Conditions created by the pandemic, such as isolation, economic stress, and community trauma, are all proven to negatively impact a child’s ability to thrive. It is vitally important that young children and their parents and caregivers receive the interventions necessary to support their mental health during this critical time.
Young children under age 5 can — and do — suffer from mental health conditions. These conditions are difficult for providers to identify and address because young children handle emotional experiences and traumatic events differently from adults and older children. During these early years a child’s brain is developing more rapidly than at any other
point in their life. Very young children are also uniquely dependent on the adults in their lives to meet their social-emotional needs and bounce back from stressful experiences. Thus, interventions must focus on caregivers to provide a nurturing, loving relationship that encourages the child’s social-emotional growth and supports the foundational brain development that will enable them to flourish.
Using information gathered from program data of early-childhood and family serving programs, interviews with state leaders and program administrators and staff and relevant literature, this report seeks to describe the wide range of community-based promotion, prevention and early identification and intervention programs for California infants, toddlers and preschoolers.
This paper focuses on community-based programs in California supporting infants, toddlers, and preschoolers’ social-emotional health, as well as their goals, service models, and funding sources. In community-based programs, care and support are delivered in spaces children and their families frequent and allow families to play an active role in their delivery. Community-based services are distinct from clinical mental health services, such as the new dyadic care Medi-Cal benefit, which, in addition to community-based services, are an essential part of the mental health system for young children. Services at the community level might look like facilitated playgroups, parenting support classes or mental health consultation for early care and education providers, among others. These programs are uniquely positioned to help families overcome barriers to mental health care access, and they can connect families and educators with more intensive health, mental health, or early intervention services as needed. Community-based programs are also most likely to reach families from historically marginalized communities, including immigrant and low-income families of color.
Existing programs for young children are often limited by a lack of resources, lack of workforce and lack of public understanding and political will. New state and federal funding in response to the pandemic have the potential to wrap culturally relevant, trauma-informed services and systems around infants, toddlers, and preschoolers. California, under the leadership of its Surgeon General, has set a bold goal of reducing Adverse Childhood Experiences (ACEs) and toxic stress by half in one generation. An increasing number of policy changes show the California Governor and legislature’s growing commitment to support mental health, and funding is increasingly being provided to mental health services for children and youth. However, more must be done to ensure that these investments reach our youngest children in community-based settings that offer critical opportunities for prevention and early supports.
This report recommends a multilayered approach that builds on the work that has already been done to promote protective factors to reduce the effects of toxic stress and ACEs that were exacerbated by the pandemic. California must braid funding sources, create system-level coordination, and ensure every community offers broad prevention efforts to support caregivers and young children.
Recommendations include:
California children and families are under significant stress, both from the COVID-19 pandemic and from other underlying issues, like poverty, racism and other forms of trauma. As parents and children increasingly return to work and school, experts predict that children and families may begin to realize the full extent of the trauma and toxic stress they have experienced related to the pandemic. Child development experts anticipate increased acting-out behaviors, separation anxiety and inconsolable sadness as children have their routines upended and experience shifts in their relationships and time spent with adults. A recent poll conducted by Education Trust-West and partners found that 70 percent of parents are worried about their family’s mental health.1 Other research suggests that many more young children are experiencing high levels of social and emotional difficulties than do in non-pandemic times.2
Even before the pandemic, young children across the state were dealing with the effects of toxic stress at levels not often appreciated by the general public. Forty-two percent of California children have experienced at least one Adverse Childhood Experience (ACE).3 ACEs are specific types of adversity, including physical and emotional abuse, neglect, and household dysfunction, which have been studied and shown to affect later health outcomes. Experiencing multiple ACEs, as well as external factors like racism and community violence, can cause toxic stress in children with long-lasting impacts on health and well-being.4 California’s Surgeon General and Governor have called the high prevalence of ACEs in California a public health crisis.5 ACEs, like the COVID-19 pandemic, disproportionately affect families of color and those with low income, and differences in exposure reflect broader societal patterns of racial discrimination and economic inequalities. The ongoing pandemic has the potential to exacerbate ACEs in young children’s lives and introduce new ones, all while deepening existing inequalities.6 In time, we will have a better understanding of the effects of the pandemic on children’s health and development, but today it seems clear that these trends have been worsened by increased family isolation, stress, joblessness and illness.
The brain development of infants and toddlers is more rapid and foundational than that of any other age group. Babies’ earliest relationships and experiences shape the architecture of their brain, creating a foundation on which future development and learning unfolds.7 Successfully preventing and treating mental health concerns among young children requires a different approach than when serving older children, adolescents or adults. That approach includes a focus on the caregivers—the healthy development of children requires nurturing relationships with adults, and the emotional well-being of young children is directly tied to the functioning of their caregivers and families. Caregiver stress, poor mental health, poverty, domestic violence or substance abuse can significantly impact young children’s mental health and interfere with development, with a potential cascade of long-term effects in later years.8 To effectively serve the family and the child, it is important that services be culturally relevant, accessible and available in locations that are comfortable to the family.
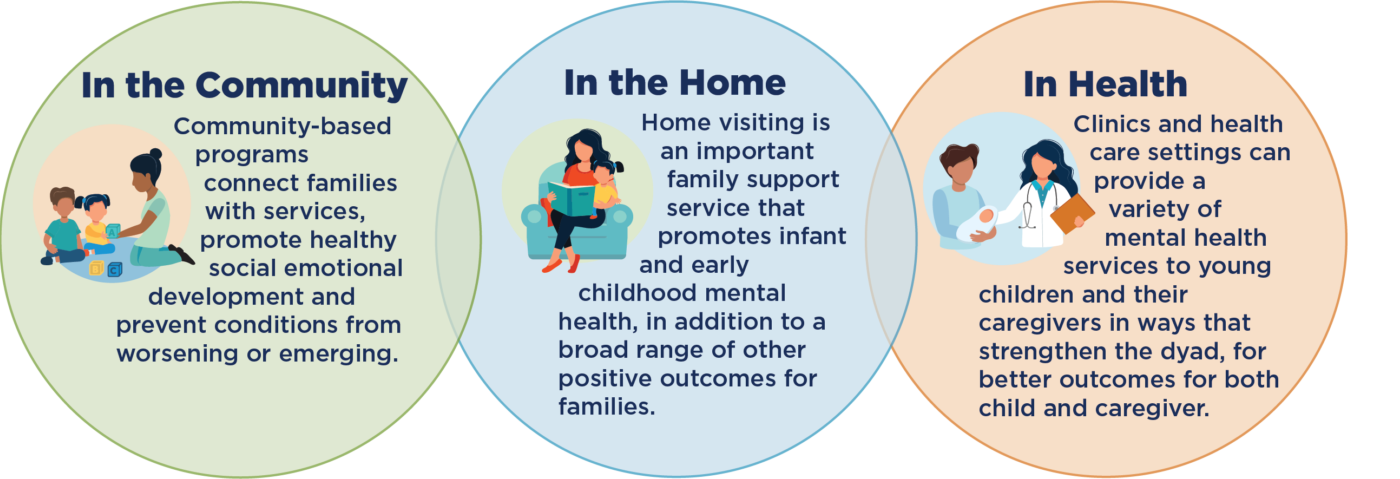
FIGURE: PROMOTING MENTAL HEALTH IN THE SETTINGS MOST COMFORTABLE TO FAMILIES
Although not often understood or recognized, young children can suffer from significant mental health conditions. At least 8 – 10 percent of children under age 5 experience clinically significant and impairing mental health problems, including emotional, behavioral and social relationship concerns.9 Young children respond to and process emotional experiences and traumatic events differently from adults and older children, making it more challenging to diagnose these concerns or understand them.10 11 For these reasons, wide-reaching systems that screen for early childhood mental health conditions, assess family well-being and link families to trauma-informed programs like Child-Parent Psychotherapy, Parent-Child Interaction Therapy (PCIT) and others can have significantly positive impacts.
The field of Infant and Early Childhood Mental Health (IECMH) is focused on supporting the early relationships between very young children with their parents and other caregivers so children can have the early experiences and foundational brain development that enable them to flourish. IECMH promotes creating stimulating early opportunities, reducing the amount of toxic stress, cultivating caring relationships with parents and other caregivers and increasing protective factors for both children and families.
IMPORTANCE OF COMMUNITY-BASED SETTINGS
IECMH services run the continuum from promotion to prevention, to developmentally appropriate assessment and diagnosis, to treatment and maintenance. These services may be delivered in a variety of settings, including the clinic, the home and in community-based settings.12 A growing body of work underscores the importance of community-level strategies, including two-generational programs that strengthen and elevate positive social norms, to heal trauma and promote resilience and assets at the community level.13
Community-based programs are uniquely positioned to help families overcome barriers to mental health care access, and they can connect families and educators with more intensive health, mental health, or developmental support, consultation or referrals to early intervention services.14 Early intervention services might include: follow-up assessments, screening for developmental and behavioral delays, family counseling and home visits, nutrition services, occupational or physical therapy, care coordination, speech and language services, special instruction, audiology or vision services.
Community-based IECMH services are generally not yet funded through traditional medical systems, though the state’s Medicaid program, Medi-Cal, is moving towards increased partnerships with community-based services through its reform effort, CalAIM. CalAIM seeks to shift the Medi-Cal program through whole-person care approaches, requiring managed care plans to collaborate with community-based partners to address member health and social needs.15 Such approaches may be particularly important in the effort to reduce toxic stress and heal communities affected by systemic racism and other traumas.16
To date, there has been no description of community-based programs that aim to support young children’s social-emotional health in California. This paper seeks to provide a description of these types of programs in California, their goals, service models, and funding sources.17
Methods
This report seeks to describe a wide range of promotion, prevention and early identification and intervention programs aimed to improve the social-emotional health of infants, toddlers and preschoolers in California community-based settings. It includes programs specifically focused on an early childhood population, and generally excludes programs that address populations otherwise defined but that may include children (e.g., programs for homeless families). Included programs primarily serve young children and families in community-based settings (examples include early care and education (ECE) centers18, family friend and neighbor care, preschools and family resource centers) and exclude services that are primarily delivered in clinics, hospitals, pediatric offices or the home.19
The data sources drawn from here include:
There is no single data source that allows for a comprehensive catalog of these services and programs across the state, and this report does not provide an exhaustive list of all programs along the promotion, prevention and early identification continuum that serve young children and their families. Our analysis focuses on programs that were initiated and/or funded by county First 5 commissions and/or county mental or behavioral health departments administering MHSA funds.
HOME VISITING AND EARLY CHILDHOOD MENTAL HEALTH
Home visiting is an important family support service that promotes infant and early childhood mental health, in addition to a broad range of other positive outcomes for families. Most early childhood home visiting models connect new and expectant parents with a designated support person, such as a nurse or early childhood specialist, who provides services in the home. Home visitors provide families with information, support and referrals to community resources and services, promote parent and child health, home safety, food security and positive parenting.22 Home visiting programs are available to some families in most counties in California and operate through various funding streams including CalWORKs, federal Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV) dollars, state general funds and First 5 Proposition 10 dollars.23 24 Providing supportive services in the home is a powerful way to support families, including the mental health and social-emotional development of parent and child. The home-based nature of home visiting programs makes them distinct from the other interventions described in this paper.
29This analysis identified 50 IECMH programs in 33 counties across the state. These IECMH programs represent a patchwork of approaches, with few examples of overarching comprehensive services for young children. They are varied, with different goals and audiences, initiated by different needs, research and funding availability. For example, many of the Infant and Early Childhood Mental Health Consultation (IECMHC) programs included in this analysis have operated for many years, corresponding with the release of research that raised awareness about child care and preschool expulsions and suspensions. Other program leaders reported that programs were initiated out of a concern about ACEs and trauma, and are designed to increase trauma-informed practice and/or broader community-based approaches.
Through this analysis, we do not have sufficient information to comprehensively describe the reach of these programs in terms of children or families served; programs vary widely with respect to target audience and data collecting methodologies. Based on stakeholder interviews, some counties reported reaching a significant proportion of child-serving organizations through broad-based prevention programs. Costlier models, like IECMHC, are often unable to reach large portions of the 0 to 5 population. One exception is San Francisco County, which includes all city-funded child care programs through a robust program that is funded jointly by multiple city and county agencies, including MHSA funds.
For the purposes of this report, we have broken county programs into four broad categories in order to distinguish their goals and approaches: Broad prevention scope; Caregiver protective factors; ECE supports; and IECMH consultation. In some cases, programs bridge these categories. See Appendix A for a table of all programs reviewed for this analysis.
Broad Prevention Scope: These programs aim to improve social-emotional well-being of young children, responsiveness and emotional attunement of parents/caregivers and ECE providers through broad communications and widely available screening services.25 Stakeholders mentioned that these programs may be effective in reducing family or ECE provider reluctance to seek services to address child behavior. In some counties, there is a robust effort to reach a wide range of families with these programs. For example, programs in Solano, Sonoma and Yolo are aimed to blanket the community with mental health resources.26 Solano County’s Partnership for Early Access for Kids (PEAK) provided education and training for parents and providers, including pediatricians and home visitors, about the signs of mental health concerns in children and how to screen for developmental and social-emotional issues.27 Yolo, San Luis Obispo and Sonoma Counties operate access and linkage programs that connect families to a wide range of services and screen for social-emotional concerns.
These efforts are similar in approach to those supported by California’s Office of the Surgeon General and Department of Health Care Services (DHCS), which recently initiated a series of funding opportunities towards the goal of reducing ACEs by half in a generation. One of these is a $30.8 million grant program to build and strengthen Networks of Care, which are intended to provide a network of services to respond to ACEs and toxic stress. Grantees include collaborations of health care and social service systems and providers. In Yolo County, the Network of Care grantee is its Help Me Grow program, jointly funded by First 5 Yolo and County of Yolo MHSA. This broad-based network identifies and works to mitigate ACEs and build resiliency. Other counties are using the Network of Care grant to build broad prevention efforts. For example, First 5 Kern was awarded an NOC grant, which will help enhance the resiliency of residents throughout the county by providing trauma-informed care and connect with local community partners to meet the social-emotional needs of families experiencing stress, including social and cultural isolation and racism.
Caregiver Protective Factors: A number of programs across the state are intended to strengthen all or some of the protective factors among parents and caregivers.28 The Incredible Years and Triple P are evidence-based models intended to strengthen these factors and improve the parent/child dyad, and we found many examples of programs using these models in community-based settings. In Contra Costa, Los Angeles, San Diego, Santa Cruz, Solano and Sonoma Counties, Triple P is offered widely to families with young children. In some rural counties in our analysis, we found the same goals of improving caregiver resilience provided in playgroup settings, which may require less travel across large geographies for isolated families. In Mono and Humboldt Counties, for example, playgroups are specifically intended to reduce the isolation of new parents and provide linkages to needed supports and parent education. First 5 Humboldt supports four endorsed Infant-Family and Early Childhood Mental Health Specialists to travel to 20 playgroups across the county on a regular basis. 29 The playgroups are hosted and led by community-based organizations and provide leadership opportunities for parents. The specialists answer questions about child development and behavior, conduct informal and formal screenings of children’s development, provide resource and referral assistance, provide parent education workshops and conduct assessments at the request of parents or caregivers. More intensive support is provided to families on an as-needed basis via office and/or home visits.
ECE Supports: In several counties, we identified programs that support the ECE field by reducing teacher stress, improving reflective practice, increasing positive learning approaches, expanding awareness of trauma and reducing mental health care stigma. In recent surveys, 30 – 40 percent of early educators reported high levels of depressive symptoms and anxiety indicating the need for increased access to mental health services. Furthermore, as pandemic stresses have led to additional behavioral and emotional needs among children, early educators also report the need for increased support and training on children’s behavioral and emotional development.30 31 Many ECE support programs have similar goals as those designed for parents and primary caregivers, but are tailored to support the early care and education field. For example, Monterey County has implemented small reflective groups for ECE educators, including groups for administrators, focused on protective factors, trauma response, prevention and healing. San Mateo County has been facilitating learning circles for ECE providers since the beginning of the COVID-19 pandemic, which it has found to be so effective that it plans to continue them beyond the emergency.
IECMH Consultation: Related to but distinct from the category of ECE supports, several communities administer a nationally-recognized model known as Infant and Early Childhood Mental Health Consultation (IECMHC). The Georgetown Center of Excellence for Infant & Early Childhood Mental Health Consultation defines IECMHC as, “a prevention-based approach that pairs a mental health consultant with adults who work with infants and young children in the different settings where they learn and grow, such as child care, preschool, home visiting, early intervention and their home.”32
The development and implementation of programs like IECMHC have emerged from both a growing understanding of the importance of promoting positive early childhood mental health and an increased recognition of expulsions and suspensions in preschools over the last 15 years. In 2005, a Yale University study found that young children were expelled at a rate far higher than children in K-12 schools. The study found that Black children were much more likely to be expelled than Latino and white children and that boys were expelled at a rate of 4.5 times higher than girls.33
IECMHC has been identified as a way to address rates of suspension and expulsion as it is an evidence-based practice to improve children’s social-emotional well-being.34 35 Research suggests IECMHC reduces challenging behaviors and improves social skills and self-regulation among children. It also improves providers’ social-emotional support to young children and classroom climate. Emerging evidence suggests IECMHC may have impacts on parents and families such as missing less time at work or school to address childcare issues and enhancing their abilities to advocate for their children after consultation. Another preliminary finding is improved teacher job satisfaction.36 Given these results, IECMHC has gained traction across the country. California’s Master Plan for Early Learning and Care calls for access to IECMHC as a strategy to eliminate bias and inequitable practices in ECE settings.37 According to the National Center for Children in Poverty, Medicaid pays for early childhood mental health specialists to address child mental health needs in ECE programs in 35 states.38
We identified 16 IECMHC county-level programs through our analysis that make IECMHC available to multiple ECE programs, though three of these have been discontinued due to a lack of funding. (See Appendix A for a full list of programs included in this analysis.) In several counties, IECMHC is provided as part of local Quality Counts initiatives, to increase the quality of ECE settings. As noted above, San Francisco County offers some level of IECMHC to all city-funded ECE programs, based on indicators of need, as well as Family Resource Centers, homeless and domestic violence shelters and substance use disorder treatment programs, through a collaboration between several city and county departments, and involving all levels of staff including administrators. IECMHC and related mental health services are required services at Head Start programs in California and the rest of the country. We also found a few other providers that have found mechanisms to provide IECMHC, including Kidango and CCRC.
Based on conversations with state and county leaders, we focused this analysis on funding sources that are directed at the local level; no statewide funding source was identified. Relevant funding sources include MHSA Prevention and Early Intervention (PEI), Innovation (INN), and First 5 funding, though those were not the only funding sources noted by interviewees. (See page 14 for a description of MHSA funding and its applicability to early childhood mental health). The majority of non-clinical early childhood development programs reviewed were funded under the PEI component of the MHSA. Across counties, leaders described a scarcity of resources in the face of large demand and overall need for services.
Overall, MHSA PEI and INN were described by counties as “game changers” that allow them to begin assisting young children and intervening in a way that can help prevent a future diagnosable mental health condition. “I just want to say that having the Innovation and Prevention and Early Intervention [programs] is such a big change from what we knew mental health was before — that you had to be really sick to get services,” said one county MHSA administrator. “Having the opportunity to do prevention and early intervention on the mental health side has been a game changer for [people who] in the past we could not serve, that we had to turn away because they did not meet our medical necessity criteria. MHSA has been the opportunity [to] prevent people from really getting sick and needing a higher level of care. So to me, that’s been a great thing.”
Counties must use 51 percent of the PEI Fund to serve individuals who are 25 years of age or younger. Programs that serve parents, caregivers or family members with the goal of addressing mental health outcomes for children at risk of or with early onset of mental health challenges can count as part of this requirement. However, MHSA county departments are not currently required to prioritize or address the needs of children ages 0 to 5 specifically, despite the rapid brain development and vulnerability of young children. Further, while some programs predominantly serve young children and their families, the counties interviewed did not have mechanisms for reporting on budget, utilization or outcomes for the 0 to 5 age range, specifically.39 Based on an analysis of PEI funding of community-based IECMH programs in nine counties, county expenditures were generally low, with eight of the nine counties spending less than 10 percent of PEI on these programs (see Appendix C for more information).
MHSA INN funding has different reporting requirements and may support untested, promising programs. It serves as a testing ground to adapt or evaluate the effectiveness of promising programs in new settings, with goals of improving quality, access and collaboration.40 In some instances, such as First Step to Success in Imperial County and Peapod in Mono County, programs have been piloted as INN and transitioned to PEI at the end of the program period.
Other INN programs that are not specific to young children test approaches to improving service access for underserved or harder-to-reach groups, such as migrant workers, Native American and other communities of color, and those living in rural areas. For example, a new INN project in Ventura County, Nuestra Cultura Cura, is working with Latino-serving organizations throughout the county to understand what factors influence mental health care and how to adapt programs to better address community needs.
First 5 county agencies, focused solely on the needs of children ages 0 to 5 and their families, have flexibility to determine how to invest their funds to best serve the community, though their funding source (a state tobacco tax) is declining. In several counties, IECMH programs are the product of partnerships between the county mental health department and the First 5 county commission (23 of the 50 included in this analysis). These partnerships take many forms but, in many cases, the First 5 initiated, developed or designed the program that is now funded by MHSA, and in some cases is also administering the services.41 For example, in Amador County, the First 5 Executive Director and Program Coordinator designed the county’s IECMH consultation program. Through a contract with county mental health and funded by PEI, First 5 identifies and contracts with licensed mental health professionals to provide the services. In Orange County, First 5 allocated seed money to initiate an Early Childhood Mental Health collaborative out of an interest in learning more about reducing the number of children being expelled from preschool programs and to pilot an IECMH consultation program for staff and leadership of ECE centers (see sidebar for more information on this program). Riverside County uses a variety of funding strategies to serve families with young children, including MHSA PEI, Medi-Cal and First 5 funding. First 5 contracts with Riverside University Health System – Behavioral Health so that it has additional funding to braid with MHSA to serve the 0 to 5 population.
Several other examples of early childhood prevention and early intervention programs rely solely on First 5 or other funding sources. First 5 San Mateo has been solely funding IECMH consultation since 1999, is expanding to family child care centers, and is increasing other ECE supports it has found to be effective. First 5 Monterey’s programs are also entirely First 5 funded, and it is implementing on-site mental health consultation in center-based programs beginning this fiscal year. This effort will support COVID-19 recovery of children, families and ECE providers and builds on a 12-year initiative of on-site technical assistance to child care centers to enhance overall program quality through relationship-based and reflective work with administrators and all program staff.
In other counties, IECMH programs have been discontinued in the last several years as a result of declining First 5 funding and a lack of other funding sources. Across several interviews, stakeholders described a lack of prioritization of early childhood needs by local MHSA decision-makers, leading them to pursue other funding sources. Motivated by the need for consultation services, the Child Care Resource Center (CCRC) now offers an IECMH consultation program in several ECE sites within Los Angeles county, and is hoping to expand the program to sites in San Bernardino. The program has no dedicated external funding source. CCRC is actively seeking other sources of funding, and has been unsuccessful in procuring MHSA funds.
Another funding opportunity for consultation programs exists at the provider level, as a result of a recently passed bill. AB 2698 (Rubio), passed in 2019, created a new adjustment factor for providers who contract with the state to care for children with a child care subsidy. The adjustment factor can increase the size of a contract by a factor of .05 and applies to all children enrolled in the classroom or family child care home setting where services are provided.42 In other words, an ECE provider who has a state contract of $100,000 would be able to use $5,000 of the contract to pay for staffing and other costs associated with consultation services. Kidango, one of the sponsors of AB 2698, leverages this funding source to provide consultation in its centers. A mental health consultant visits their classrooms once a week for two to three hours to observe the classrooms and meet with staff and caregivers. Because of its size and scale, and its historical commitment to providing mental health services onsite, Kidango is able to make mental health consultants available year-round, rather than just when an issue in a classroom emerges.
Specific regulations detailing how to use this provision have not yet been published, however, and many providers may not yet know about this adjustment factor for IECMHC, or how to use it. Further, this approach requires that child care administrators recognize the importance of IECMHC for their staff and can identify a mental health provider who is trained and available to provide the services. Another significant challenge is that the adjustment factor may not be high enough to fully cover the costs of implementing IECMHC in many communities.43
MHSA FUNDING MECHANICS AND USE FOR EARLY CHILDHOOD MENTAL HEALTH:
The Mental Health Services Act (MHSA) was established via ballot initiative Proposition 63 in 2005. It contained a 1 percent tax on personal income over $1 million to supplement mental health activities across a broad set of services. Funds from the MHSA are allocated to counties for expenditures via local plans that contain five required categories: Community Services and Supports (CSS), Prevention and Early Intervention (PEI), Innovation (INN), Capital Facilities and Technological Needs (CF/TN) and Workforce Education and Training (WET).44 MHSA is a predominant funding source for child mental health programs in California, second only to Medi-Cal.45 MHSA components are locally defined, allowing for significant variation at the local level.
The PEI category is designed to fund services that promote wellness, foster health and prevent people from languishing from untreated mental illness. Local departments are required to have at least one PEI program in each of the following categories: 1) Prevention; 2) Early Intervention; 3) Outreach for increasing recognition of early signs of mental illness (may be a stand-alone program or a strategy within another program); 4) Access and linkage to treatment (may be a stand-alone program or a strategy within another program); 5) Stigma and discrimination reduction programs.
PEI regulations will soon be adjusted as a result of the passage of SB 1004 (Wiener) in 2018. Among other things, that bill requires counties to allocate a portion of their PEI funds towards additional priorities, including childhood trauma prevention and early intervention. SB 1004 also calls for the expansion of high-quality MHSA PEI programs, including those utilizing community-defined practices that have a focus on serving historically marginalized communities.46 A report from the Mental Health Services Oversight & Accountability Commission (MHSOAC) in response to SB 1004 directives is expected in Winter 2021.
Start Well: A Multisector 0-8 Collaborative in Orange County
Start Well Orange County is an infant and early childhood mental health consultation program developed in Orange County and is the first of its kind in the state. The project is the result of a pilot and research project and formation of an Early Childhood Mental Health Collaborative, both initiated by First 5 Orange County. The Collaborative comprises the OC Regional Center, Children’s Home Society of California, OC Health Care Agency, OC Department of Education, and OC Association for the Education of Young Children.
The members of the collaborative conducted a local survey of over 700 ECE providers to better understand their needs and experiences caring for children with challenging behaviors. One of their findings was that young children under age five were being expelled from centers at high rates for what was described as bad behavior. Based on these findings, the Collaborative planned, piloted, and evaluated the Start Well program. The Collaborative presented its effectiveness to the Mental Health Services Act Board and has since sustained the effective model through PEI dollars.
Start Well staff employ two evidence-based practices, the Pyramid Model and the Infant/Early Childhood Mental Health Consultation Model, to work collaboratively with ECE provider staff to implement a multi-tiered system to support every child’s social and emotional development. Through consultation, observation, and supporting communities of practice, Start Well ensures knowledge and fidelity of the models, and sustainability. Centers receive ongoing support through “communities of practice,” where both alumni and current program participants are invited to participate in knowledge exchange.
California’s current behavioral health workforce meets less than a third of the need, according to the Steinberg Institute.47 The workforce is not evenly distributed across the geography of the state, nor does it reflect the racial/ethnic diversity of the state’s population.48 For children with Medi-Cal insurance, availability of behavioral health providers is limited even further, as not all providers accept insurance, including Medi-Cal, and many providers are not trained to work with young children.49 The lack of trained professionals, both licensed and unlicensed, with expertise in early childhood mental health development limits county programs and poses a significant barrier to meeting child and family needs, particularly families of color in the post-pandemic era.
These findings were corroborated and expanded upon throughout our interviews. County leaders noted the general lack of mental health professionals, as well as those with specific training in infant and early childhood mental health and social-emotional development. Rural communities, in particular, described struggling with workforce shortages and transportation issues that limit service availability for families in hard-to-reach areas. Hiring and retaining clinicians and other mental health staff who are multilingual and/or share racial, ethnic and cultural identities with families was another common challenge identified.
Stakeholders identified a number of reasons for these shortages, including low pay and a general lack of specialization. County departments of mental health and community-based organizations compete with private practices that offer more competitive compensation, a dynamic described as particularly challenging since the emergence of COVID-19. As one county behavioral health service director reflected, “It seems like there’s more opportunities for people to explore positions that are in the private market and utilize telehealth.” Moreover, stakeholders highlighted the lack of early childhood courses or requirements at institutes for higher education that train social workers and other clinical staff.50 This is a significant gap for employers seeking to fill roles that interface with families.
To address this gap, several counties are investing in training programs. In Yolo County, one-time MHSA funding put a cohort of providers through the Napa Infant-Parent Mental Health Fellowship program at UC Davis. In order to receive their scholarship, providers pledge a certain number of service hours to work with children identified by their Help Me Grow system as needing additional support. San Bernardino has a Cultural Competency Advisory Committee that develops workforce education and training activities, with a focus on its rural communities. One of the programs develops pathways for students in public schools to interest them in the behavioral health profession and serve their community.
Training programs or other incentives for rural communities may be particularly important. Smaller counties and those with vast rural areas described having a limited mental health workforce and a challenge attracting child mental health specialists to the region. One MHSA coordinator said it would be impossible for a child psychologist or psychiatrist to sustain a practice in her county, given what would be an insufficient demand for their services. Some stakeholders highlighted the need for loan repayment programs to incentivize clinicians to move to those communities. The UC San Francisco Infancy/Early Childhood Mental Health Consortium is working with 11 rural northern counties to offer an array of professional development opportunities to seed and support an IECMH workforce in that region.51 The initiative is focusing on organizations that serve the Native American/Tribal population to reduce isolation and heal historical trauma. The Consortium is funded through a Substance Abuse and Mental Health Services Administration (SAMHSA) grant, which ends in 2023.
In addition to training programs to add to the clinical workforce, a number of counties are investing in training programs for child care and preschool teachers, to promote their ability to work with children and families experiencing trauma or other stressors. For example, for 10 years, Monterey has offered early educators countywide an Infant and Family Early Childhood Mental Health Training Series on the importance of infant mental health and trauma-informed/healing-centered work. The training has a Spanish language cohort, which invites the participation of diverse early educators including center-based and in-home educators.

Some counties are working to strengthen their child mental health workforce by reviewing their internal policies and practices related to diversity, equity and inclusion. Doing so was described as fundamental to connecting with and building out networks of culturally-specific providers. “Administratively, there is a recognition that we need to hire people who are the community: The community are us, and we are the community,” said one county administrator. “[Our] staff live in the community, grew up in the community, went to [the] schools [and] received the services that we provide...that is foundationally a shift that has occurred and a commitment on the part of our departments.”
Other counties are developing models to uplift and fund culturally-specific communities in planning and implementing mental health programs and overcoming barriers to building a more representative mental health workforce. Ventura County, for example, has a large migrant indigenous community from Oaxaca, Mexico, that has been engaged in the workforce through the MHSA-funded Healing the Soul, which has a professional development component.52 As one county administrator said, “We’ve always taken the stance that we need to learn.[Working] with individuals who are from [the community], they were really clear we don’t have the language to talk about mental health. [We’re] really honoring them to teach us what it’s like to live in their world and within the defining of what their world is; not the Western concept of illness and individualism, when really we’re talking about [health of] the community and the family.”
RECENT PUBLIC INVESTMENTS AND COMMITMENTS TO IMPROVING EARLY CHILDHOOD MENTAL HEALTH.
State and federal policymakers have made recent commitments to mental health services that will benefit children. Together, these policy changes represent major windows of opportunity to build a more comprehensive, intentional system to target public investments in the kinds of services and approaches that have been demonstrated to yield long-term outcomes, reduce stress, and mitigate the impacts of ACEs. Recent policy changes that may support child, family and community mental health and wellness include:
Across the landscape of early childhood mental health, California, and the country, this is a moment of change. The pandemic has made the public more aware of mental health needs, including those of families with young children and of infants and toddlers themselves. Family isolation, economic stress, and community trauma — conditions that increased as a result of the pandemic — all negatively impact a child’s ability to thrive. Interventions that build the capacity of parents and caregivers to respond to a child’s dynamic emotional state and strengthen the bond between them show unique promise at reducing adversity and addressing not only the child’s social-emotional needs, but also those of the adults in their lives. As noted by the Surgeon General: “Californians clearly recognize what the science has been revealing over the past several decades: that adversity, especially in the early years of life, can dramatically curtail health and life opportunities.”60
Through this research, we found a range of services available at the county level to address IECMH using varied approaches, reflecting different goals and the availability of funding. Though often limited in their ability to reach families widely, they offer different types of services, including a broad prevention scope, strengthened caregiver protective factors, ECE supports, and infant and early childhood mental health consultation. Based on the interviews conducted for this analysis, IECMH programs are limited at the county level in their reach and capacity by a lack of resources, lack of workforce and lack of leadership.
In some counties, these programs are a part of, or linked to, other systems that serve families, like Help Me Grow, which links families to services in the community, or Quality Counts, which aims to strengthen the quality of ECE settings. But more can be done at the systems level to create holistic approaches to serving families through a range of program types and settings. Systems-level planning and implementation of programs have the ability to reach families early and in the settings that are most comfortable for them, as a means to heal community-experienced trauma. This will require a commitment to whole child approaches at the state and county levels, and significant leadership.
New state and federal funding offer the opportunity to wrap culturally relevant, trauma-informed services and systems around families. Governor Gavin Newsom’s Administration and the California legislature have demonstrated a commitment to addressing mental health concerns and helping families recover from the stresses of the pandemic. Under the leadership of the state’s Surgeon General, California has made enormous gains in assessing the needs of young children with ACEs and setting a bold goal of reducing ACEs and toxic stress by half in one generation. Moreover, the state’s new Children and Youth Behavioral Health Initiative dedicates $4 billion to transforming mental health services for children and youth ages 0 to 25. These and other policy changes and commitments indicate a growing understanding for the need to support young children’s social-emotional development. (See above for more information about recent relevant investments).

However, additional policy changes are needed to ensure that the unique and critical needs of infants, toddlers and young children are addressed. California should pursue a multilayered approach to promoting protective factors for young children, their parents and caretakers to stem the tide of accumulating toxic stress from the pandemic. Through the blending of funding sources and approaches, and systems-level coordination, California can ensure that every county offers community-wide broad prevention efforts, supports for caregivers and ECE providers to build protective factors and reduce stigma, and provide consultation services in all ECE settings. Specifically, we recommend:
APPENDIX A: TABLE OF IECMH COMMUNITY-BASED PROGRAMS
Programs were identified through a review of county MHSA reports, First 5 program data, and other web research. Interviews were conducted with representatives from 20 counties including First 5 and county mental or behavioral health department staff to provide additional information about identified programs for our analysis. The programs described in the table below represent the results of this research, but it is not an exhaustive list of all community-based programs that benefit the social-emotional development of young children. We note which programs are supported by MHSA and/or First 5 funding sources, though programs may have other funding sources as well.
County | Included early childhood mental health programs | Program Category | Program receives MHSA Funding | Program receives First 5 Funding | Short description |
|---|---|---|---|---|---|
Alameda | Early Childhood (birth-8) Mental Health Prevention: Blue Skies Mental Wellness Team (MWT) | Consultation | X | Consultation for home visiting programs | |
Alameda | CSEFEL trainings | ECE support | X | ECE provider trainings and support groups for family childcare | |
Alameda | Consultation training model (discontinued)* | Consultation | IECMH consultation for ECE providers | ||
Amador | Early Childhood Mental Health Consultation | Consultation | X | IECMH consultation for ECE providers | |
Butte | Center CARE project | Consultation | X | IECMH consultation modified for a rural setting | |
Colusa | MHSA Infant to 5 Program | Consultation, Caregiver protective factors | X | IECMH consultation model with parenting class component | |
Contra Costa | Triple P – Positive Parenting Program | Caregiver protective factors | X | X | Parent classes offered throughout the county |
Contra Costa | First Five of Contra Costa ECMHC (discontinued)* | Consultation | IECMH consultation program for ECE providers | ||
Del Norte | Text 2 Grow | Caregiver protective factors | X | Text-based parent support system | |
Del Norte | Incredible Years (Dina Dinosaur) | Caregiver protective factors, Broad prevention scope | X | Dina Dinosaur curriculum provided at preschool sites, collaborative of multiple agencies | |
El Dorado | Community Hubs | Caregiver protective factors | X** | X | Family strengthening protective factors trainings in community hubs |
Glenn | Strengthening Families Program | Caregiver protective factors | X | Evidence-based program that develops parenting skills | |
Humboldt | ECMHC for playgroups | Caregiver protective factors | X | Consultants travel to playgroups around the county | |
Humboldt | SEEDS program (discontinued)* | Consultation | IECMH consultation for ECE providers including Tribal centers | ||
Imperial | First Step to Success | Broad prevention scope | X | Screening and referrals, relationship-building between schools and mental health providers | |
Imperial | The Incredible Years | Caregiver protective factors | X | Parenting education groups | |
Los Angeles | Incredible Years (IY) | Caregiver protective factors | X | Group-based parenting program | |
Los Angeles | Making Parenting a Pleasure (MPAP) | Caregiver protective factors | X | Group-based parenting program | |
Los Angeles | Families Over Coming Under Stress for Early Childhood (FOCUS-EC) | Caregiver protective factors | X | Home-based family resiliency training for military families | |
Los Angeles | Triple P – Positive Parenting Program: Levels 2 and 3 | Caregiver protective factors | X | Light-touch parenting classes | |
Los Angeles | SEEDS (Strategies for Enhancing Early Developmental Success) | ECE support, Consultation, Caregiver protective factors | X | Trauma-informed programs for parents and professionals | |
Marin | Early Childhood Mental Health Consultation | Consultation | X | X | IECMH consultation in ECE centers |
Mono | Peapod Program | Caregiver protective factors | X | X | Playgroup program aimed at reducing social isolation |
Monterey | ECMHC program | ECE support, Consultation | X | On-site technical assistance for ECE providers with consultative team, expanding to offer consultation | |
Nevada | Teaching Pro-Social Skills in the Schools | ECE support | X | Trainings for ECE providers focused on social-emotional skills | |
Orange | StartWell program | Consultation, ECE support | X | IECMH consultation and provider trainings for family and center-based ECE providers | |
Orange | School Readiness (Prevention Track 1 and Early Intervention "Connect the Tots" Track 2) | Caregiver protective factors, ECE support | X | Education, training and coaching for caregivers and ECE providers | |
Riverside | Preschool 0-5: Nurturing Parenting | Caregiver protective factors | X | X | Short-term parent groups |
Riverside | Preschool 0-5: Education Equip and Support (EES) | Caregiver protective factors | X | X | Parenting support for families with children with emotional challenges |
Riverside | Preschool 0-5: Growing Healthy Minds | Broad prevention scope, ECE support | X | X | Screening and referral resources, parenting tips, videos on topics related to emotional development |
Sacramento | Quality Child Care Collaborative (QCCC) | Consultation | X | X | IECMH consultation for family child care and centers-based providers in high needs areas |
San Bernardino | Preschool PEI Program (PPP) | Consultation, Caregiver protective factors, ECE support | X | Caregiver and ECE provider trainings, classroom supports by psychologists | |
San Diego | Triple P – Positive Parenting Program | Caregiver protective factors | X | Parenting classes for parents with children in Head Start, Early Head Start | |
San Francisco | Early Childhood Mental Health Consultation Initiative | Consultation | X | X | Multi-agency collaborative offering consultation to child-serving organizations |
San Luis Obispo | Developmental Screening Partnership | Broad prevention scope | X | Screenings administered by parents and by ECE providers | |
San Mateo | Early Childhood Community Team | Consultation, Caregiver protective factors | X | IECMH consultation, community referrals | |
San Mateo | ECMHC | Consultation | X | IECMH consultation linked to Quality Counts | |
San Mateo | Learning circles for ECE providers | ECE support | X | Virtual learning opportunities | |
Santa Barbara | The Great Beginnings | Caregiver protective factors, Broad prevention scope | X | Prevention and early intervention mental health services, focused on Latinx populations | |
Santa Clara | Support for Parents (includes Positive Parenting Program - Levels 2-5 and NFP) | Caregiver protective factors | X | Parenting classes offered throughout the county | |
Santa Clara | Services for Children 0-5 (part of KIDCONNECTIONS NETWORK) | Broad prevention scope | X | X | Screening, assessment and service linkages |
Santa Cruz | Triple P – Positive Parenting Program | Caregiver protective factors | X | Group-based parenting program | |
Shasta | Triple P – Positive Parenting Program | Caregiver protective factors | X | X | Group-based parenting program |
Siskiyou | Nurturing Parenting Program | Caregiver protective factors | X | X | Trauma-informed parenting education |
Solano | A Better Way, Triple P – Positive Parenting Program | Caregiver protective factors | X | X | Parenting training offered by multiple service providers in various settings |
Solano | Early Childhood-Partnership for Early Access for Kids (PEAK) Program-(Ages 0-5) (discontinued)* | Broad prevention scope | X | X | Mental health screenings and educational sessions on screening tools and other topics for parents and providers |
Sonoma | Child Parent Institute (CPI) - Triple P – Positive Parenting Program | Caregiver protective factors | X | Parent education in individual and group formats | |
Sonoma | La Luz Center - Your Community, Your Health / Tu Comunidad, Tu Salud (NEW for 21-25) | Broad prevention scope, Caregiver protective factors | X | Family workshops and referrals provided by community health workers | |
Sonoma | Early Learning Institute (ELI) - Watch Me Grow | Broad prevention scope, Caregiver protective factors | X | Screenings and navigation services | |
Yolo | ECMH Access & Linkage program | Broad prevention scope | X | X | Links families to screenings, offers developmental playgroups, and refers families to services |
* These programs were discontinued for various reasons, including a scarcity of resources and sustainable funding sources.
** El Dorado’s program was funded through a combination of funding including a five-year Mental Health Services Act Innovation grant. The MSHA funding has been discontinued, though the program continues with First 5 funding.
APPENDIX B: LIST OF INTERVIEWED STAKEHOLDERS
The authors thank the many experts who were interviewed for this report and those who offered comments and insights on the drafts. They include:
Michelle Blakely, Deputy Director, First 5 San Mateo
Francis Calero, ECMHCI Lead Coordinator, San Francisco Department of Public Health
Hilary Carson, MHSA Innovations Program Administrator, Ventura County Behavioral Health
Ellen Cervantes, Vice President and Chief Operating Officer, CCRC
Gina Daleiden, Executive Director, First 5 Yolo
Molly DesBaillets, MA, Executive Director First 5 Mono County
Barbara DuBransky, Deputy Director of Programs, First 5 Riverside
Lindsay Dunckel, Early Learning Coordinator, First 5 Sacramento
Michelle Dusick, MHSA Administrative Manager, Department of Behavioral Health, San Bernardino County
Ruth Fernandez, Executive Director, First 5 Contra Costa
Trina Frazier, Assistant Superintendent of Student Services, Fresno County Superintendent of Schools
Liliana Gonzalez, Help Me Grow Program Coordinator, First 5 Contra Costa
Kim Goll, President/Chief Executive Officer, First 5 Orange
Tammi Graham, Executive Director, First 5 Riverside
Amanda Greenberg, Program Manager, Mono County Behavioral Health
Mary Ann Hansen, Executive Director, First 5 Humboldt
Michele Harris, Executive Director, First 5 Solano
Beth Hoch, Training Administrator, First 5 Alameda
Susan L. Holt, LMFT, Deputy Director, Clinical Operations (All4Youth Program), Department of Behavioral Health, County of Fresno
Barbara Ivins, Co-Project Director, Infancy and Early Childhood Mental Health Consortium, UCSF Benioff Children's Hospital Oakland
Yael Koenig, LCSW, Deputy Director, Behavioral Health Services, Children, Youth and Families, Health & Human Services Agency, County of San Diego
Melinda Konoske, Consultant, MK Consulting
Melissa Ladrech, LMFT, Mental Health Services Act Coordinator, Department of Health Services: Behavioral Health Division, Sonoma County
Mark Lawrenz, LCSW, Division Manager, Prevention and Intervention Behavioral Health Services, Orange County Health Care Agency
Los Angeles County Department of Mental Health
Nina Machado, Executive Director, First 5 Amador
Ingrid Mezquita, Director, Office Of Early Care And Education, San Francisco Human Services Agency
Danyte S. Mockus-Valenzuela, PhD, MPH, Unit Manager, Behavioral Health Services – Prevention and Community Engagement, Health & Human Services Agency, County of San Diego
Scott Moore, Chief Executive Officer, Kidango
Kelly Morehouse-Smith, Family Well-Being Director, CCRC
Dina Olivas, LCSW, Youth & Family Division Chief, Ventura County Behavioral Health
Sarah O’Rourke, Program Manager, First 5 Orange
Leticia Plancarte-Garcia, MSW, MPA, Director, Imperial County Behavioral Health Services
Camilla Rand, Deputy Director, First 5 Contra Costa
Bhuvana Rao, PhD, Division Manager, Office of Suicide Prevention, Behavioral Health Services, Orange County Health Care Agency
Beth Reeves-Fortney, Director of Programs, First 5 Monterey
Kirstin Reinsberg, Interim Director, Infant-Parent Program, UCSF Department of Psychiatry and Behavioral Sciences
Riverside University Health System - Behavioral Health (RUHS-BH)
Leticia Sanchez, Vice President of Programs, First 5 Orange
Hoda Shawky, Maternal/Early Childhood Consultant, Hoda Shawky Consulting
Yvonne Suarez, Deputy Director of Administration, First 5 Riverside
Min Tan, Director of School Based Mental Health Services, San Francisco Department of Public Health
Raquel Williams, LCSW, Program Manager, Prevention and Intervention Behavioral Health Services, Orange County Health Care Agency
Rosario Williams, Family Well-Being Manager, CCRC
Maria Wyatt, MA, Behavioral Health Manager, Imperial County Behavioral Health Services - Children’s Programs: Vista Sands, MHSA PEI and Innovation
Theresa Zighera, Interim Executive Director, First 5 San Francisco
APPENDIX C: COUNTY MHSA PEI ANALYSIS
We analyzed data on MHSA PEI expenditures in nine counties to ascertain the percentage of PEI funds that are dedicated to community-based services for children ages 0 to 5 and their families.
Our analysis included interviews, written correspondence, and a review of MHSA Annual Reports and Three-Year Plans. Through these data sources, we identified:
(1) Estimates of total MHSA PEI expenditures for the county (see column B in table below);
(2) MHSA PEI programs that are non-clinical and primarily serving children ages 0 to 5 (see column C); and
(3) Estimates of expenditures for this subset of MHSA PEI programs (column D).
We calculated the percent of funding dedicated to non-clinical programs focused on young children and their families by dividing FY19/20 MHSA PEI Expenditures (column B) by FY19/20 Non-Clinical 0-5 Program Expenditures (column D). The result is presented in column E.
County (Column A) | FY19/20 MHSA PEI Expenditures (Column B) | Non-Clinical Early Childhood Mental Health Programs (Column C) | FY19/20 Non-Clinical 0-5 Program Expenditures (Column D) | Percent of MHSA PEI funding for non-clinical early childhood mental health program (Column E) |
|---|---|---|---|---|
Fresno | $18,427,926 | N/A | N/A | 0.0% |
Imperial | $1,707,375 | Incredible Years, First Step to Success | $899,997 | 52.7% |
Los Angeles | $244,100,000 | Triple P, Incredible Years, Families Over Coming Under Stress, Making Parenting a Pleasure | N/A* | N/A |
Mono | $474,000 | Peapod | $40,000 | 8.4% |
Orange** | $42,355,334 | School Readiness, StartWell | $2,429,533 | 5.2% |
Riverside | $23,441,987 | Parent Education and Support (inclusive of the Preschool 0-5 Programs) | $1,956,692 | 8.3% |
San Bernardino | $21,096,774 | Preschool PEI Program | $377,725 | 1.6% |
San Diego | $26,761,835*** | Triple P – Positive Parenting Program | $1,106,050 | 4.1% |
Sonoma | $4,355,019**** | Child Parent Institute Triple P, Early Learning Institute Watch Me Grow, and La Luz Center Tu Comunidad, Tu Salud | $321,000 | 7.4% |
Ventura***** | $6,878,533 | N/A | N/A | 0.0% |
* Expenditures for individual services not available in Los Angeles County FY21-23 MHSA Three-Year Plan
(only totals for Early Intervention and Prevention as shown on pages 97 and 113, respectively).
** As StartWell is a significant but new program addressing priorities identified in the 2018 community planning process, and will first be reported on for FY20/21, all Orange County numbers reflect FY20/21 estimates.
*** Dollar amounts represent all revenue sources, since “they are comingled within services”: MHSA, Realignment, and Federal Financial Participation (FFP) (19-20 MHSA Annual Update (p. 33)).