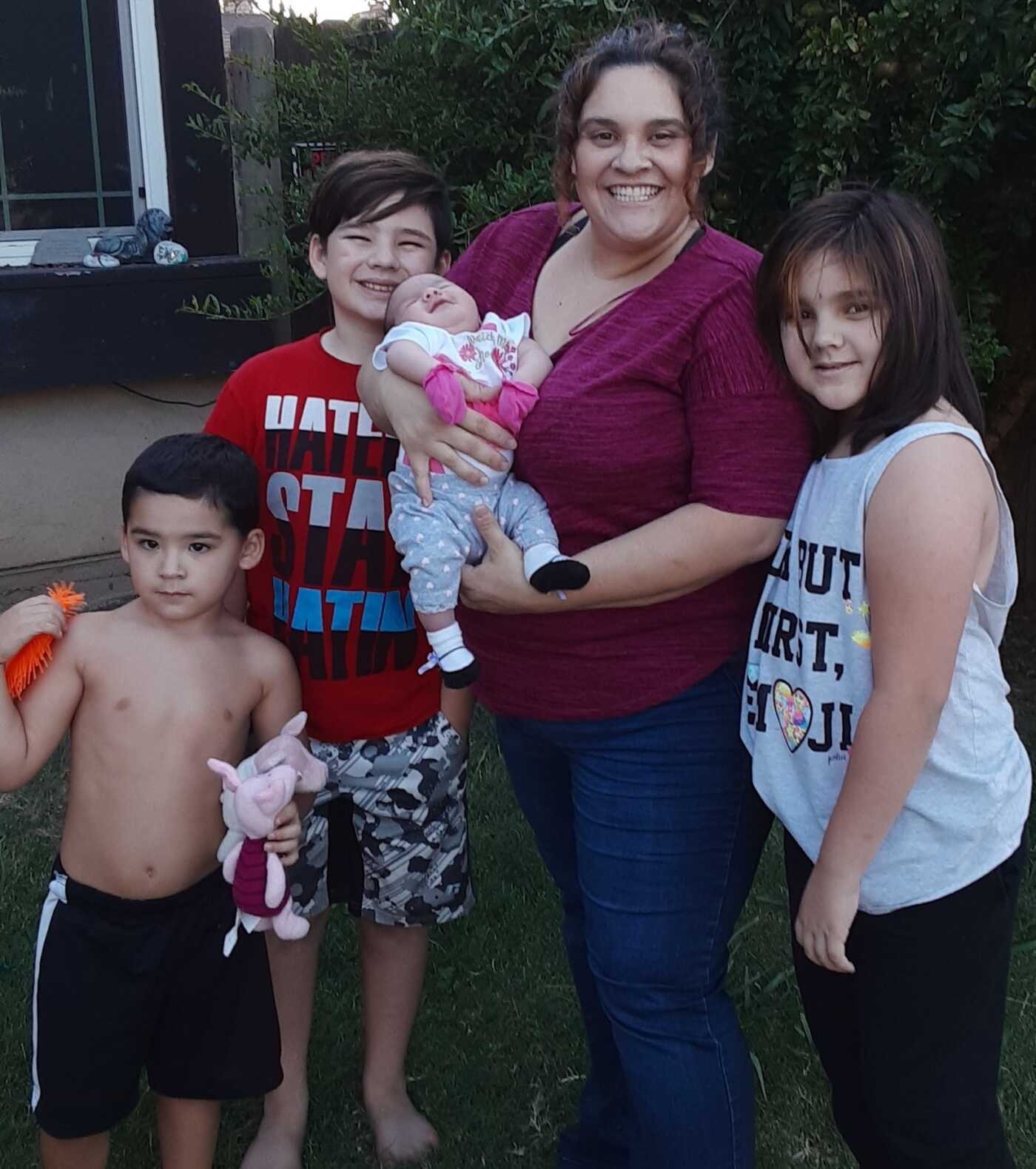
When a child shows signs of a developmental concern, getting connected to supports early is key. Leticia DeGracia, a Sacramento mother of four young children, knew this was true and took swift action when two of her children, Jaqueline and Brandon, showed symptoms of autism spectrum disorder (ASD). Despite Leticia’s determination to get answers and support, the DeGracia family journey to receive diagnoses and services was complicated.
After going through the process of securing services for her older daughter, Jaqueline, Leticia became very savvy with insurance, state laws, and ASD-related interventions. “I wanted to do anything and everything I could to help my daughter be the best that she could be,” she noted. After Leticia voiced her concerns about Jaqueline to her pediatrician, Jaqueline was referred to the Regional Center and the MIND Institute, a research center for neurodevelopmental disabilities. There, Jaqueline was diagnosed with ASD at age two and quickly gained access to many supports.
Unfortunately, the process didn’t proceed as smoothly when Leticia’s son, Brandon, began exhibiting signs of ASD a few years later.
First, Brandon’s pediatrician wanted to “wait and see” before assessing him for delays, so Leticia had to seek out the appropriate specialists. She knew having a diagnosis would give Brandon access to additional services and Medi-Cal coverage. Then, the family’s insurance changed and Leticia had to navigate a new health network that didn’t include the doctors she knew at UC Davis.
One of the biggest obstacles that Leticia faced with Brandon was that her new insurance plan didn’t have an in-network pediatric psychologist in the Sacramento area who could assess Brandon. Leticia was told that she had to drive to San Francisco to have Brandon assessed for ASD. Leticia remembers telling the insurance company, “What kind of assessment do you think he is going to have after driving two hours away?” Brandon ended up seeing a local in-network neurologist who diagnosed him with global delays, ASD, and oppositional defiant disorder. However, the family’s insurance plan and the Regional Center still needed the diagnosis to come from a pediatric psychologist.
Determined to see a pediatric psychologist closer to home, Leticia asked her grandmother to watch the kids as she spent six hours researching her options. “I was so stressed out.” Leticia recalls. “I knew there had to be a way to get this done. I was in mama bear mode. I needed to get services and I knew early intervention was the key. I knew time was ticking away.” Leticia figured out a way to see a local specialist through her job’s employee assistance plan (EAP), which allows for six behavioral health visits for her and her family at no cost. She found a pediatric psychologist at UC Davis who was contracted through the EAP to assess Brandon. “I went the back roads,” she noted.
In addition to barriers with referrals and private insurance, Leticia also has faced many challenges applying for Medi-Cal for Jacqueline and Brandon. Paperwork and filing errors at the Medi-Cal office slowed down the process while Leticia continued to pay for expensive copays out of pocket even though it was financially challenging for the family.
Jaqueline and Brandon (now ages 8 and 4) are both receiving services and doing well. However, the ongoing COVID-19 pandemic has increased stress about job and insurance stability for the DeGracias, as well as many other families in California.
Our EII flowchart shows the complexity that families like Leticia’s often navigate to get services. Leticia is an incredibly resourceful mother, but families shouldn’t have to spend days or weeks researching options and workarounds. “There are many hurdles us parents encounter,” noted Leticia reflecting on her experience seeking services for her children. “It’s not right.”